A
5-years-old girl presented with progressive abdominal distension since past one
month. There was no associated history of jaundice, fever, vomiting or
bowel complaints. she was anicteric and mild pallor was noted.
Laboratory values were: Hb- 10.9 g/dL, total bilirubin-1.1 mg/dL, SGPT-38
IU/L, SGOT-35 IU/L.
On examination a large, soft, non-tender lump was palpable in the right hypochondrium, extending to the right iliac fossa and umbilical region. The lump had a smooth surface and was continuous with liver dullness. She had non palpable spleen, no ascites and all other systems were found to be normal
DISCUSSION:
Choledochal cysts are classified according to the Todani modification of the original Alonso-Ley classification. five groups are identified. Type I is a fusiform dilatation of the extra hepatic bile duct, as was found in our patient. Type II is a single extrahepatic diverticulum. Type III is a dilatation of the intraduodenal portion of the bile duct. Type IV consists of two subtypes: IVa which is combined intra- and extrahepatic dilatation and IVb which is multiple extrahepatic cysts only. Type V is also known as Caroli’s disease and consists of cystic dilatation of the intrahepatic biliary system. It is also associated with hepatic fibrosis.
The etiology of choledochal cysts remains unproven but an anomalous pancreaticobiliary junction has been reported in choledochal cyst disease. Babbit proposed a theory that suggests a high insertion of the bile duct into the pancreatic duct allowing pancreatic enzymes to reflux into the bile duct. This causes inflammation, weakening and fibrosis of the bile duct and the distal obstruction leads to progressive dilatation of the biliary tree. Children present with the classic triad of abdominal mass, abdominal pain and jaundice.
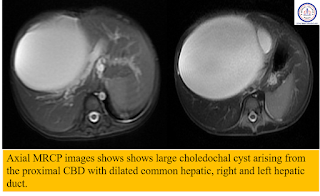
Laboratory tests have not been proven to be useful in establishing a diagnosis and it has been shown that hepatic transaminase, bilirubin and white cell count were normal in up to 50% of patients at time of diagnosis. Imaging however is essential in making a diagnosis. Ultrasound and CT are useful for detecting cysts, but differentiation from other fluid collections and confirmation of the biliary origin of the cyst can sometimes be difficult. Direct contrast cholangiography is used to define extent of involvement and visualize the remaining biliary tree. Contrast cholangiography is invasive though, and magnetic resonance cholangiography (MRCP) is a non-invasive technique, accurate in confirming the diagnosis of choledochal cysts and defining extent of involvement pre-operatively.
There is an increased risk of malignancy in choledochal cysts and the occurrence of cancer is most marked in adults. Type I has the highest predominance of cancer, followed by the type IV cyst. The type III cyst is the least common type harboring cancer. Most of the tumors found are adenocarcinomas, although squamous and anaplastic cell carcinomas are occasionally discovered. The most common site of occurrence is the posterior cyst wall. Prognosis is poor and most patients die within 2 years of diagnosis.
Currently total excision with reconstruction of the biliary tree by means of Roux-en-Y hepaticojejunostomy is considered to be the treatment of choice although type III cysts have been shown to respond adequately when managed with endoscopic sphincterotomy.
(Ref.Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cyst: Classification, operative procedures, review of 37 cases including cancer arising from choledochal cyst. Am J Surg. 1977;134(2):139‒169. and O'Neill JA. Choledochal Cyst. CurrProbl Surg. 1992;29(6):363‒410.)













0 Comments